One of the only retreats in the nation for HIV-infected people and their partners:
Tag Archives: health
Hepatitis C Seminar In Missoula
On Thursday, April 25th from 5:00pm-6:00pm, Open Aid Alliance is offering the first of three community seminars on hepatitis C. The first presentation will feature Dr. Rebecca Kinney. Dr. Kinney completed medical school at Mount Sinai School of Medicine in New York City, and did her residency at Family Medicine Residency of Idaho in Boise. She is a family physician specializing in infectious diseases, with specific expertise in hepatitis C. This presentation will provide an overview of hepatitis C infection, transmission, and recommendations for testing. All three seminars are free and open to the public.
Thursday, April 25th, 2013
5:00pm-6:00pm
MCT Center for the Performing Arts (use the Main Street entrance)
Room 302
For more information, call Open Aid Alliance at 406.543.4770 or email stephanie@openaidalliance.org
Please join us for this opportunity to expand your knowledge of hepatitis C
Young Gay Men’s Retreat April 12-14
Women’s Health Stats For Montana
WOMEN’S HEALTH IN MONTANA (DHHS REGION VIII) Female Population of MONTANA
Total state population: 989,415 (492,748 females; 496,667 males)
Health Status (Age-adjusted§ percent of adult females)
In poor general health: 4.4%
Activity limitation due to poor phys/mental health: 8.9%
No natural teeth: 5.4% Sources: 2010, BRFSS
Access to Care (Age-adjusted§ percent of adult females) No health insurance coverage (under 65): 21.2%
No personal doctor or primary care physician: 79.2% Saw a dentist in past year: 61.5%
Fact sheets are now available for each of the 50 states and the District of Columbia. Each fact sheet presents a snapshot of demographic characteristics as well as a variety of health status indicators for females within the area. These include:
· Health Status
· Access to Care
· Health Conditions and Risk Factors
· Preventive Services and Screenings
· Mortality
· Prenatal Care and Pregnancy Risk
· Birth Outcomes
· Sexually Transmitted Infections
· Violence and Abuse
· Mental Health and
· Teen Health
For complete Montana stats, click here.
Related articles
- Suicide rate among Montana’s senior citizens outpaces national figure (billingsgazette.com)
- Millions of Americans Have an STD: Report (news.health.com)
- New study reveals sex to be pleasurable with or without use of a condom or lubricant (eurekalert.org)
- Few pregnant women treated for sexually transmitted infections (scienceblog.com)
- Women’s health must be priority for state health exchange marketplaces, new report says (eurekalert.org)
How The Sequester Hits Montana
Here’s the link to the effects of the sequester for Montana.
One of the great “benefits” being the inability to pay for 117,000 HIV tests- now free for any Montana resident. And there’s more besides.
http://www.whitehouse.gov/sites/default/files/docs/sequester-factsheets/Montana.pdf
Related articles
- The Sequester is Coming! (blogs.barrons.com)
- Sequester Could Lead To Massive Cuts In HIV Testing, Treatment (pinkbananaworld.com)
- Montana passes law allowing motorists to eat animals they kill with cars (metro.co.uk)
- Wyoming officials: White House report does little to alleviate ‘sequester’ confusion (trib.com)
Train To Do HIV Rapid Testing and Counseling!
Here’s an opportunity to do some good:
FREE 3-day Training!!!
.
.
Click here for more info: CTRS Training February 2013
And if you’re interested in becoming a testing associate for AIDS Outreach, please email info@aidsoutreachmt.org
Related articles
- Michigan Awards Nearly $2.5M For HIV Prevention (detroit.cbslocal.com)
- Rollout of provider-initiated HIV testing (africanpress.me)
- Multiple factors affect HIV prognosis, study shows (yaledailynews.com)
- Need for education in the prison system imperative (kaieteurnewsonline.com)
- Rapid HIV testing first (theage.com.au)
The Girl Effect
The infographic below was created by the Girl Effect which is a movement about leveraging the unique potential of adolescent girls to end poverty for themselves, their families and the world. It highlights the problem of child marriage which leads to pregnancy and childbirth which can be fatal for young girls- not to mention damaging to a country’s economy.
Related articles
- Nike Foundation launches new girleffect.org (nikeinc.com)
- The Girl Effect (neilperkin.typepad.com)
- Women in social entrepreneurship (socialbusinessrevolution.com)
HIV Patients Lose More Years To Smoking Than HIV
Bad news for people with HIV who smoke: you’re losing twice as many years of your life by continuing your habit. And that’s not all. You’re also going to die at three times the rate of non-smokers with HIV….
Among HIV patients receiving well-organized care with free access to antiretroviral therapy, those who smoke lose more years of life to smoking than to HIV, according to a Danish study published in Clinical Infectious Diseases and available online. The findings highlight the importance of smoking cessation efforts in the long-term, integrated care of patients infected with HIV.
Marie Helleberg, MD, of Copenhagen University Hospital and colleagues estimated the effect of smoking on mortality, risk of death, and life expectancy, and the number of life years lost to smoking compared to years lost to HIV among nearly 3,000 HIV-infected patients treated in Denmark from 1995 to 2010. They also compared mortality associated with smoking between HIV patients and the country’s background population. Where HIV care is integrated and antiretroviral therapy is available at no cost, “more than 60 percent of deaths among HIV patients are associated with smoking,” rather than HIV, Dr. Helleberg said.
Estimated life expectancy differed significantly based on smoking status. A 35-year-old HIV patient who currently smokes had a life expectancy of 62.6 years, compared to 78.4 years for a nonsmoker infected with HIV. The loss of years of life associated with smoking was twice as high as that associated with HIV among HIV-infected patients. In addition, researchers found the excess mortality of HIV-infected smokers to be three times higher than that of individuals not infected with HIV.
Quitting smoking-along with increased exercise- are the two things people with HIV can do to extend their lives and overall health. I quit over three years ago. And yeah, it’s not easy. But it’s worth it.
So if you need a New Year’s resolution, it’s staring you right in the face. And if you need help, it’s readily available here.
Read the full article at Science Daily
Related articles
- New York Life Expectancy Rises to Record 81 Years, Mayor Says (bloomberg.com)
- Clinicians Asked To Screen All Patients For HIV (dgsmith.org)
- A new treatment for AIDS? (bio230fall2010.wordpress.com)
- HIV Patients Hospitalized Less Since the Advent of Antiretrovirals (webpronews.com)
- Can You Keep HIV From Becoming AIDS? (everydayhealth.com)
- Living Longer With HIV (everydayhealth.com)
Identification of LGBT Needs in the Exam Room

A physician performs a routine checkup on a patient at the medical clinic. (Photo credit: Wikipedia)
Last time you were in an exam room, did you feel that the attending physician received all the information needed to gain an accurate perspective of your plight? Did you share everything you felt you should, no matter how personal? Did said physician even ask about anything, aside from the usual short list of inquiries we are all too familiar with in that particular setting?
If you are a physician, do you really get the answers you need from your patients? Or perhaps it is just too uncomfortable when talking about sexual health and behaviors. More likely, they do not disclose the details out of discomfort, or even fear.
LGBT persons have shown to have some unique healthcare needs, sometimes experiencing disparities in care. LGBT patients are often uncomfortable or inhibited from talking openly with healthcare providers about sexual orientation, gender identity, and sexual behaviors. Certain sexual behaviors do not automatically define that patient as LGBT, and not all LGBT patients are going to have similar sexual behaviors. Truthfully, it’s not about whether a person is a member of the LGBT community or not. It’s about the individuals choices and behaviors that could be putting their health at risk, as well as the health of others. In order to cover everyone’s needs, patients must speak openly with providers. Providers must delve into the patients behaviors and understand where the risk behavior is at for each patient. I am going to lay out a few examples, ideas, and suggestions for physicians, as well as patients.
In any healthcare position, you will find people from diverse backgrounds and lifestyles. Different interests, tastes, and mindset. The right approach will reassure patients that the provider is knowledgeable, genuine, concerned, confidential and accepting. This enables the patient to open up and discuss the very private matters of sexual behavior, often in this society a ‘taboo’ subject.
Ask the patient to tell a bit about themselves. As the patient, make sure you indulge your sexual partner(s), safe sex practices, and concerns. Some behaviors have an amount of risk attached to them that is often unknown to the patient. A physician might ask “Do you have any questions or concerns about your sexuality, sexual orientation or sexual desires?”. Use gender-neutral terms and mirror the patient’s terminology to better understand how they identify. For example, asking “do you have a partner or spouse?” “Are you currently in a relationship?” “What do you call your partner?” are all good ways to decide how the patient will identify without offending them with clinical terms which may sound cold and ‘labeled’. From here the in-depth sexual questions begin: “Are you sexually active?” “When you have sex, do you have sex with men, women or both?” “Are you and your partner monogamous?” “How many sexual partners have you had in the past year?” “Do you have vaginal sex, anal sex, or both?”. These and many more are the key to finding out just what unique needs your particular patient might have.
It is important to differentiate between sexual identity and sexual behavior. Providers need to discuss sexual behavior with patients regardless of sexual identity in order to define risk-assessment, ascertaining what activities they engage in and to learn what they are doing to prevent the transmission of disease.
And for the majority of readers, as patients we have a personal responsibility to find the courage to openly discuss in confidence all of our behaviors and desires with our doctors, nurses, therapists and counselors, etc. This is extremely important. We cannot rely on someone to read our thoughts and know the truth.
Stand up and be proud of yourself. I can almost guarantee that the person treating you has heard it all. And if they haven’t, they will soon enough.
Study: Access to HIV Services for Gay Men Worldwide Stunted By Homophobia
Global study finds homophobia, comfort with service provider, and community engagement make significant impact on access to condoms, lubricant, HIV testing, and HIV treatment
A large-scale study of gay men and other men who have sex with men (MSM), conducted by the Global Forum on MSM & HIV (MSMGF), indicates that only one third of MSM can easily access condoms, lubricant, HIV testing, and HIV treatment. Combining a multi-lingual online survey and focus group discussions, the study suggests that structural barriers like homophobia play a significant role in blocking access to HIV services for MSM, while greater comfort with service providers and community engagement are associated with higher levels of service access.
The MSMGF’s study aimed to identify barriers and facilitators that affect access to HIV services for MSM. The online survey conducted this summer included 5779 men from 165 countries. In addition, the MSMGF collaborated with African Men for Sexual Health and Rights (AMSHeR) to conduct focus group discussions with a total of 71 MSM across five cities in South Africa, Kenya, and Nigeria.
Of men who participated in the online survey, only 35% reported that condoms were easily accessible, 21% reported easy access to lubricant, 36% reported easy access to HIV testing, and 42% reported easy access to HIV treatment. Levels of access differed across low-, lower-middle-, upper-middle- and high-income countries, with reduced access to services more commonly reported in lower-income countries.
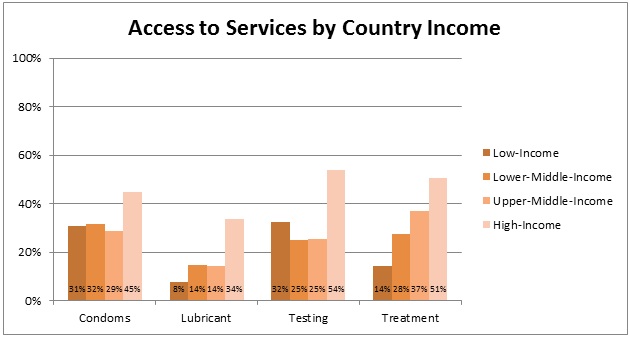 Percent of MSM reporting that condoms, lubricant, HIV testing, and HIV treatment
Percent of MSM reporting that condoms, lubricant, HIV testing, and HIV treatment
are easily accessible
(organized by country income level using World Bank country income classifications)
“Such poor levels of access at the global level are unacceptable,” said Dr. George Ayala, Executive Director of the MSMGF. “The differences in access by country income level are especially important to note as the Global Fund moves into a new funding model where countries are grouped into bands by income level. Even in upper-middle-income countries, MSM still have extremely low access to services. Without targeted funding to MSM and other key populations, the new funding model may continue to deteriorate levels of access for the groups most affected by HIV.”
The MSMGF research team also conducted analyses to identify barriers (factors associated with lower access) and facilitators (factors associated with higher access) that impact the ability of MSM to obtain condoms, lubricant, HIV testing, and HIV treatment.
Adjusting for country income, greater access to condoms, lubricants and HIV testing were associated with less homophobia, greater comfort with health providers, and more community engagement. Among participants living with HIV, higher access to HIV treatment was associated with less homophobia and greater comfort with service providers. Greater access to lubricants and greater access to HIV testing were also associated with less outness (the degree to which others know of one’s sexual orientation) and fewer negative consequences as a result of being out, respectively.
“As we collectively forge ahead into the new territory of treatment-based prevention, it is clear that many of the old challenges remain,” said Noah Metheny, Director of Policy at the MSMGF. “Addressing structural barriers remains essential to realizing the potential of HIV interventions for MSM, and it becomes more important with each new prevention and treatment option that is made available. Investments in the development of new interventions must be accompanied by efforts to increase access.”
The quantitative data from the online survey was supplemented with qualitative data from focus group discussions, helping to place barriers and facilitators in the broader context of the sexual health and lived experiences of MSM. Focus group discussion participants identified barriers and facilitators that were highly consistent with those found in the online survey, and many participants explained the ways that structural barriers at the policy, cultural, and institutional levels cascade down through the community and individual levels to block access to services for MSM.
Focus group discussion participants described how structural barriers like stigma, discrimination, and criminalization force MSM to hide their sexual behavior from health care providers, employers, landlords, teachers, and family members in order to protect themselves and maintain a minimum livelihood. The inability of MSM to reveal their sexual behavior to health care providers was linked to misdiagnosis, delayed diagnosis, and delayed treatment, leading to poor health prognosis and higher risk of transmitting HIV and other sexually transmitted infections to partners.
Conversely, focus group discussion participants explained that the negative consequences of structural barriers were moderated by the existence of safe spaces to meet other MSM, safe spaces to receive services, access to competent mental health care, and access to comprehensive health care. Participants described MSM-led community based organizations as safe spaces where they could celebrate their true selves, receive respectful and knowledgeable health care, and in some cases receive mental health services.
“The study’s findings underscore the urgent need to improve access to essential HIV services for gay men and other MSM worldwide,” said Dr. Ayala. “Interventions must both disrupt the negative effects of barriers and bolster the protective effects of facilitators. Study participants clearly indicated that community engagement and community-based organizations are central to moderating barriers and facilitating service access. Successfully addressing HIV among MSM will require a real effort to address structural barriers, and the findings from this study suggest that investing in MSM-led community-based organizations may be the best way to do that.”
Agreed. MSM-led community-based organizations must continue to work tirelessly to eliminate fear, shame, stigma and ignorance. They are all still very much with us.
And they’re killing us.
Related articles
- Why HIV Testing and Treatment Are Still Issues (dgsmith.org)
- Talking HIV (rappler.com)
- Federal panel recommends HIV testing for ‘everyone’ (bangordailynews.com)
- HIV Testing Will Now Be Covered Under Obamacare (thinkprogress.org)
- Back of the Line: The State of AIDS Among Black Gay Men in America (williamlarsonpharmd.wordpress.com)



